Patient centered care sounds like an obvious thing to aim for in healthcare, always, everywhere. However, its implementation is not always a straightforward matter. Persistent bureaucracy, increasingly complicated diagnosis, and treatment processes throw spanners in the works.
How can we ensure that the patient is the central beneficiary of the healthcare trajectory? Can AI lend a helping hand? This article discusses 8 angles of patient centered healthcare and examines the promise of AI each of them.
So what exactly is patient centered healthcare?
Patient centered care is about treating the person, not the disease. A patient should be involved in decision making about his or her own health. To accomplish this, it is important that understandable information is available, on both the disease as well as the treatment options. Furthermore, it is of great value to make the whole diagnosis and treatment trajectory as smooth as possible for a patient, for example, through timely access to care, easy transitions from one healthcare facility to another, or by offering the right amount of both emotional and physical support throughout the process.1,2
How can healthcare AI play a role in improving patient centered healthcare?
Isn’t patient centeredness rather subjective? Preferred way of interacting, diagnosis method, and optimal treatment choice can differ per patient. True, however, researchers at Harvard Medical School summarized and categorized the essence of patient centered care in eight principles. In this section, we will discuss these principles and assess the role AI can play for each of them.3
1. Respect for the patients’ values and preferences
At first glance, this might seem like an area that is reserved for humans; however, it is actually of great importance to make sure values and possible preferences play a role in AI algorithm development and implementation. What kind of output an algorithm gives can be adjusted according to what is interesting for a patient to hear. Some outputs may not be the most informative or directional information for a physician, but a patient would be very eager to know. For example, a diagnosis of Alzheimer’s disease (AD) and understanding the current phase of disease development. In case of late stage AD, this information might be less interesting for a physician as it does not lead to a change in treatment planning, but for a patient it can be extremely valuable to get a more detailed diagnosis and understand what is going on in his or her head.
Additionally, the way we treat the outcome of an algorithm and weigh it against the patient’s preferences is important as well. Physicians need to be educated on how to take the answers AI provides into account. Is it treated as a second opinion? Will the AI diagnosis be leading? And how is the diagnosis communicated to the patient? Not everyone will be happy to hear “the computer says you are healthy, so we’ll go with that”.
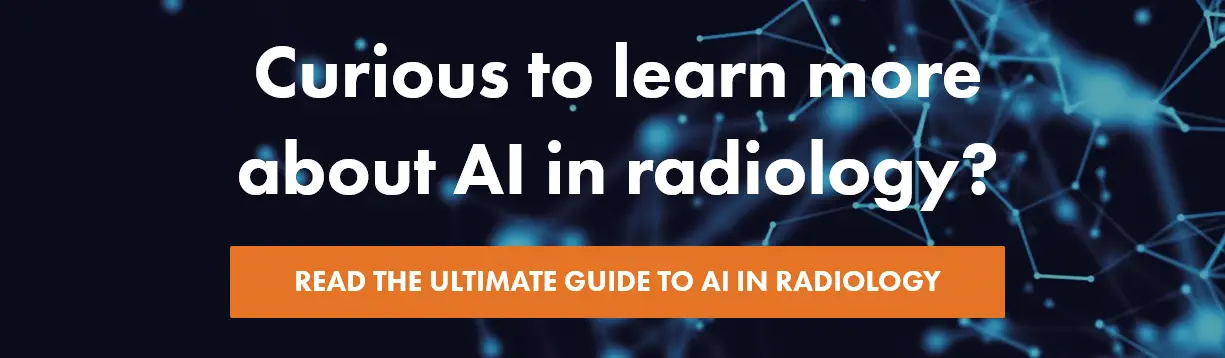
2. Coordination and integration of care
Healthcare AI is ideally suited to improve coordination of care. It is possible, for example, to train an algorithm that can predict peak hours at an emergency department and support it with admission coordination. What about software that can flag most acute cases and prioritize these patients? AI-powered integration of care also offers great opportunities. AI can play a big role in streamlining the information exchange between departments by, for instance, automatically gathering results from different patient exams and presenting these cohesively in a dashboard to be used during multidisciplinary team meetings (MDTs). Another example is the alignment of different types of care. Imagine an algorithm that has been trained on at least thousands of cases and can therefore predict how to combine chemo- and radiation therapy for the best result.
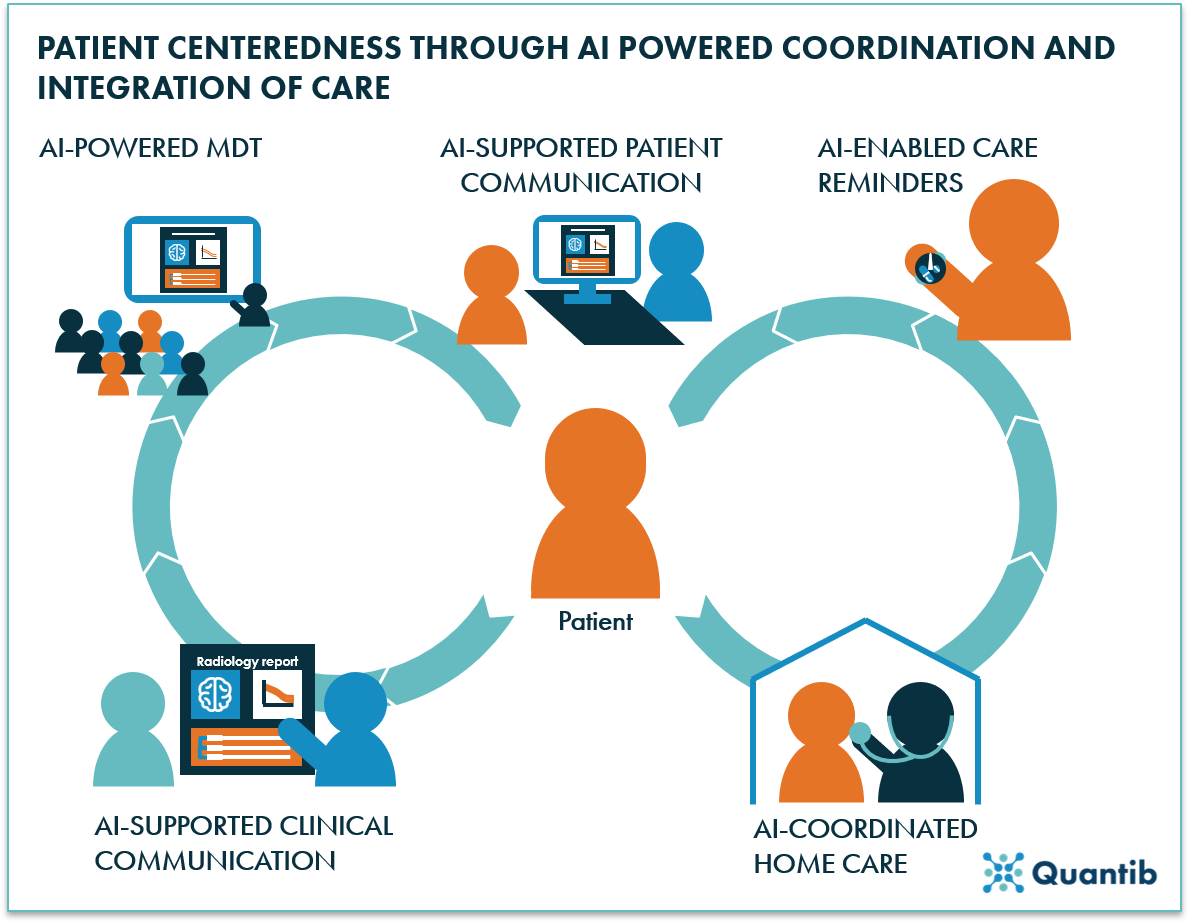
Figure 1: AI can support patient-centeredness through AI-powered coordination and AI-supported integration of care. Examples are MDTs with AI-organized information, patient communication that is supported by AI tools, patient reminders coordinated by AI software, clinical communication using reports created with AI, or AI-enabled home care.
3. Information, communication, and education
It is not without reason that information, communication, and education are mentioned in one go. Patients want to know and understand what is going on in their body and how exactly their treatment works. This requires information, but also adequate communication to educate the patient about his or her situation. AI can offer support across the board. AI could generate additional information for patients that will help them to understand their situation. For example, the creation of reference curves to show a patient that his or her brain volume is showing stronger atrophy than a healthy brain at the same age would show; or, the automated creation of a clear standardized report including explanatory images, which can support the communication with a patient.
4. Physical comfort (pain management, assistance with daily living, hospital surroundings)
Managing a patient’s pain is often an important aspect of a treatment trajectory. However, deciding on medication that will most likely lead to the best outcome is not always a straightforward exercise. In the era of big data, it is possible to use large datasets that include treatment choices and their effect, in order to train algorithms predicting what medication is most likely to benefit a specific patient. AI-powered, personalized healthcare will be able to contribute strongly to the realization of patient centered care.
5. Emotional support and alleviation of fear and anxiety
What can AI do for a patient when it comes to comfort and reassurance? Although providing emotional support is difficult for machines to master, anyone who has seen the Disney movie Big Hero 6, must remember how a giant, white, balloon-like robot manages to comfort a little kid after losing his brother. This is only an animated movie, but the concept is clear: robots that are equipped with an algorithm that constantly registers and processes the human activity around it, can determine an appropriate “caring” response - an innovation that will be achievable in the future using AI.
6. Timely access to care
A significant contribution AI can deliver is the acceleration of current healthcare processes, resulting in shorter waiting times. It is not uncommon that a patient has to wait weeks before he or she can get an MRI. AI has the potential to redesign scanning protocols, shortening scan time, and therefore enabling radiographers to scan more patients each day. Another example: AI can provide expert level knowledge at smaller hospitals and clinics. This ensures that, regardless of the healthcare setting a patient ends up in, timely quality care is guaranteed.
Figure 2: Timely access to care should be realized to guarantee patient centeredness.
7. Involvement of family and friends
For most patients, the involvement of family and friends is of great importance. This can be anything from having them present at doctors’ appointments to provide support while examination results are shared, to including them in the decision making process, or by involving them in treatment.
What opportunities does AI offer in this context? Artificial intelligence will never replace family and friends, but AI could enable close relatives to perform more care tasks instead of nurses. If a medical product can accurately measure relevant metrics and an AI healthcare algorithm can determine what treatment acts to perform, it can tell a family member what to do and keep an eye on whether it is done correctly - not that different from what an automated external defibrillator (AED) is able to do nowadays.
8. Continuity and secure transition between health care settings
Going from one hospital to another, or to a rehabilitation center, can be a challenging changeover. What can AI do to make such transitions as smooth as possible?
Anyone working in a healthcare position knows that the average number of faxes, burned CDs, or memory sticks that are being exchanged daily exceeds any other industry. This is error prone and takes precious time, while 2020 offers easier, faster, and more accurate ways to share (confidential) patient information. Of course, this should happen in a highly secure fashion; hence, a robust, well-tested, AI-enabled security system can allow for data sharing through the cloud.
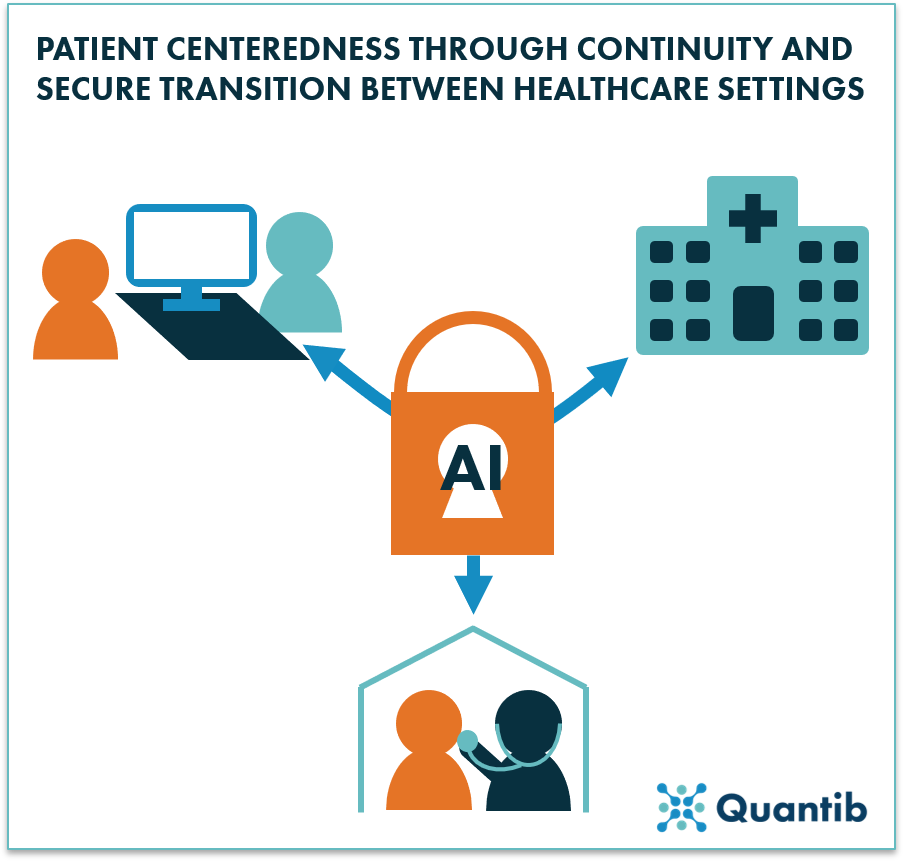
Figure 3: AI has the potential to create secure connections between various healthcare settings.
To conclude
AI can affect and add value in many areas of patient centered healthcare. It can help battle the ever-growing burden of bureaucracy and administration that healthcare is so familiar with. It can help get patients the right care at the right time.
For many of the aforementioned applications, there is still a long way to go before they are being implemented in hospitals and can bring value to the patients, but they are far from unrealistic and will be part of the future diagnostic and treatment pathway.
Bibliography
- Patient-centred care explained. (2015). Available at: https://www.betterhealth.vic.gov.au/health/servicesandsupport/patient-centred-care-explained/. (Accessed: 23rd January 2020)
- Delaney, L. J. Patient-centred care as an approach to improving health care in Australia. Collegian (2017). doi:10.1016/j.colegn.2017.02.005
- James, T. A. Transforming the Patient Experience of Health Care. (2018). Available at: https://leanforward.hms.harvard.edu/2018/04/27/transforming-the-patient-experience-of-health-care/. (Accessed: 16th January 2020)