The healthcare system is evolving and personalized healthcare is becoming increasingly important. From this perspective, each patient is unique. Therefore, it is of utmost importance to take into account as much information as possible, including that obtained from the medical images (such as tumor volumes calculated based on MRI images). However, many radiologists are already strained as it is, and adding more details to the radiology report not only takes time, but may also generate extra questions from referring clinicians. During a workday that is already overcrowded, this would lead to a significant increase in workload. Therefore, a key question to answer, especially in this era of artificial intelligence (AI) in radiology, is how to take into account and report as much relevant information as possible without overloading radiologists with even more work.
A key factor in the diagnostic workflow is communication between radiologists and referring clinicians, such as neurologists. Communication takes place in various forms at various moments - during an official multidisciplinary team meeting (MDT), or as a quick question for advice in the hallway, and anything in between. Improving this essential part of the diagnostic chain has great potential to reduce the heavy workload of both radiologists and referring physicians, while including more details on the patient in the decision-making process. This is especially the case when part of the data collection and report preparation can be automated. Implementing such changes can eventually lead to improved patient care, since this aspect greatly depends on the quality of the diagnostic process. One of the key communication elements in the diagnostic chain is the radiology report - containing all relevant information derived from the medical images of the patient in question. Improving this important information document can create great gains for all physicians involved as well as the patient. But what exactly are the potential benefits?
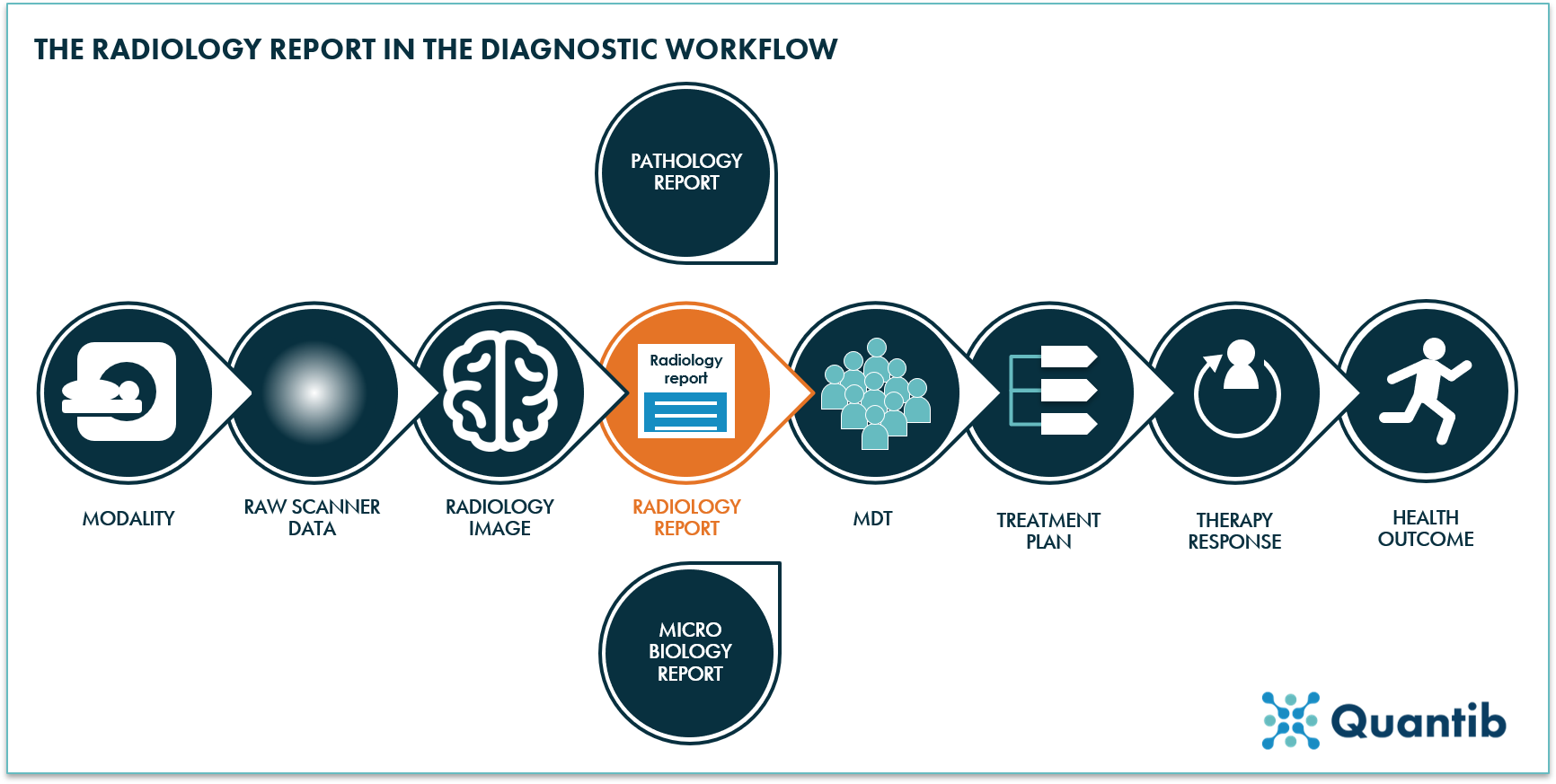
Figure 1: An overview of the diagnostic workflow with the radiology report as a key element.
4 benefits of an optimized radiology report
A radiology report can be optimized in may ways, for example, by adding (more) structure to the report, incorporating key images, including (more) quantitative data, or by presenting this data in easily comprehensible graphs. Many professional radiological societies already recommend including several standardized elements to enhance radiologist reporting and to reduce inter-reader variation. However, radiology reports can be improved further. Doing this will help to realize the following benefits:
1. More efficient communication with referring physicians using optimized radiology reports
Structure in any kind of report is key to effectively communicate the main findings while minimizing variation between radiologists. Clinicians can easily spot the requested information without having to read the whole report. Additionally, being able to put the patient results into context at one glance will not only accelerate the interpretation of the report, but also provide detailed information, valuable for getting a diagnosis. For example, a radiology report that includes reference data allowing to compare the patient’s results to that of a normative population, can offer more quality context.
2. Improved MDT communication using optimized radiology reports
Multidisciplinary team meetings can become very long if many clinicians are involved and all of them have a lengthy contribution to share. Imagine just needing a few graphs, immediately providing the key insights deduced from the medical scans, and speeding up the information transfer during an MDT. For example, deciding on how to manage the patient can be enabled by providing immediate overview of the (disease) development over time. Radiology reports that include a synopsis of prior exams can greatly contribute to the decision making during MDTs.
3. Refined patient communication through optimized radiology reports
A radiology report can be hard to understand for a patient. This is not surprising, because the document is not directly addressed to patients. Its goal is to communicate radiology findings to referring physicians. However, what if all parties involved could use one document only to communicate important findings? Radiologists, clinicians, and patients would all have access to the same information without someone copying it from one (digital) spot to another. This does not necessarily mean the complete report is written in layman’s terms, but at least part of it should explain the situation in such a way that someone without a medical background can understand its meaning. This has great potential to avoid miscommunications. Not to mention the feeling of being in control it would give the patient if he or she feels that all available information is shared with them in a clear and understandable way. Something that can be achieved by presenting the data in a structured way and providing insights in clear graphs. It goes without saying that it is of tremendous added value to have a physician discussing the findings and the radiology report with a patient personally as well. Most likely, it is undesirable to omit this step in any diagnosis process.
4. Better basis for algorithm training using radiology reports
Standardization of the data collection has one major additional benefit: it will make accurate algorithm development much easier. Organized data is key for the training of well-functioning AI algorithms. Clear and complete documentation of the data will help the programmer in the selection of the data needed for training. This is of utmost importance as inadequate selection can cause algorithm bias.
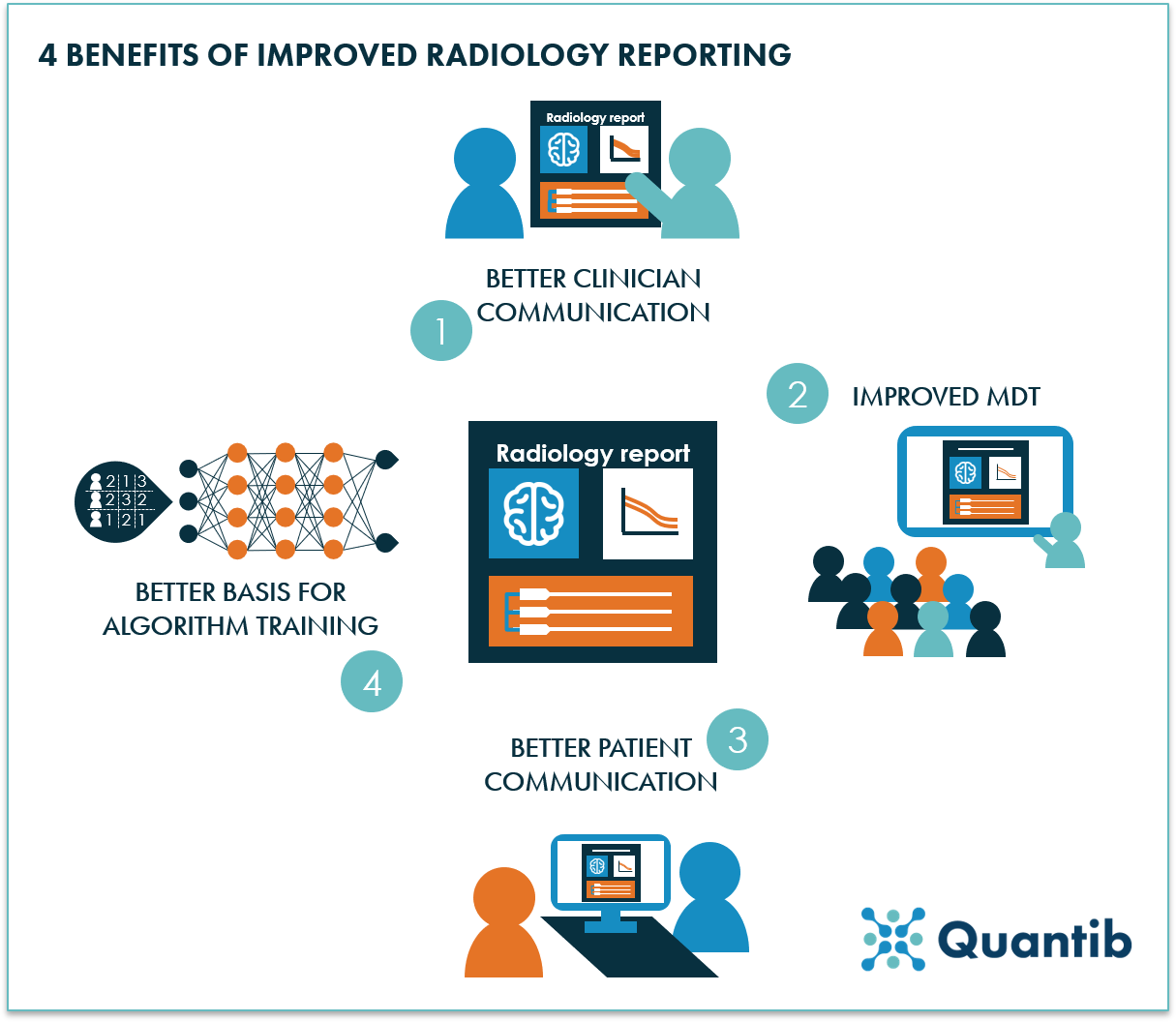
Figure 2: 4 benefits of optimized radiology reporting: better clinician communication, improved multidisciplinary team meetings, refined patient communication, and a better basis for algorithm training.
Eager to implement optimized radiology reporting?
It is clear that we can benefit in various aspects from optimized radiology reports. Some of the benefits mentioned above may already contribute to a streamlined diagnostic workflow in your institute. Others still offer large opportunities. To ensure the optimization of radiology reports will not lead to an increasingly complicated and time-consuming task for radiologists, techniques such as artificial intelligence may prove to be of substantial added value in the future. Ready to upgrade your radiology reports? Stay tuned for our blog on How to advance your radiology reporting!