It is only natural that urologists and physicians want to make the process of diagnosing possible prostate cancer (PCa) as easy and comfortable as possible for their patients. This, alongside providing support and allowing them to make their own informed decisions, is the basis of patient centeredness1,2.
However, the clinical pathway for PCa diagnosis can be long and tedious. The number of tests required to get to an accurate diagnosis can be vast, which most likely will have a large toll on the patient, physically, due to the risks involved with invasive testing, mentally and financially.
Therefore, supporting patients during these insecure times can be challenging. The general outline is clear: be empathetic and provide easy-to-understand information. But how can you become that physician that makes getting diagnosed with prostate cancer a bearable experience for your patient?
This blog post will provide handles to physicians to support and reassure their patients in every step of the clinical pathway for PCa diagnosis.
Current prostate cancer pathway and how to improve the patient experience
Having the clinical pathway for prostate cancer diagnosis in mind, we will walk you through things you can do as a urologist to support and reassure your patient in throughout the diagnostic and treatment process.
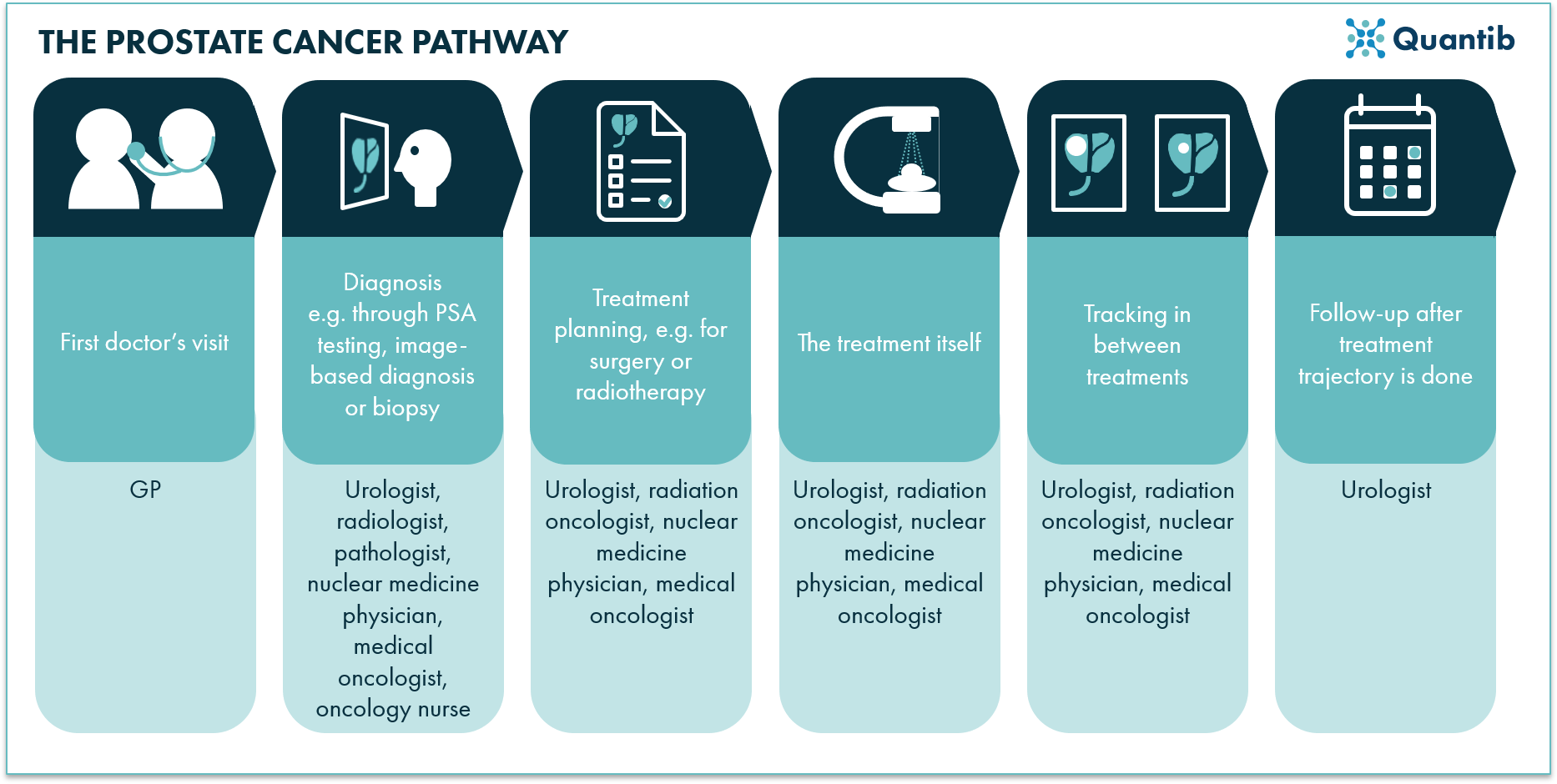
Figure 1: Summarized overview of the clinical pathway for prostate cancer diagnosis.
Optimized resources for prostate cancer patients
Firstly, we will discuss handles that will help you deliver the most value possible and that can be applied throughout the most if not the whole prostate cancer pathway.
Carefully explain concepts, procedures and treatments
A thorough explanation of the different concepts involved in urology may be essential for the patient, especially when it is the first time he may be in contact with the specialty. When it comes to testing, for example, it is important to explain what the test is, how to prepare and what the results may be.
This will enable patients to know what to expect from the procedures they are about to undergo, and be more comfortable with the processes. Simultaneously, it will reduce chances of invalid testing, as the patient would be thoroughly prepared.
What assets can support the conversation and help explain difficult procedures, all risks and details involved?
- Infographics for the prostate cancer pathway
Infographics are a great way of explaining difficult concepts in a digestible manner to patients3. For example, the process of a Prostate Specific Antigen (PSA) test, who should take it and what are the possible outcomes: low or raised PSA, can be briefly explained in an infographic presenting the procedure in a visual way.
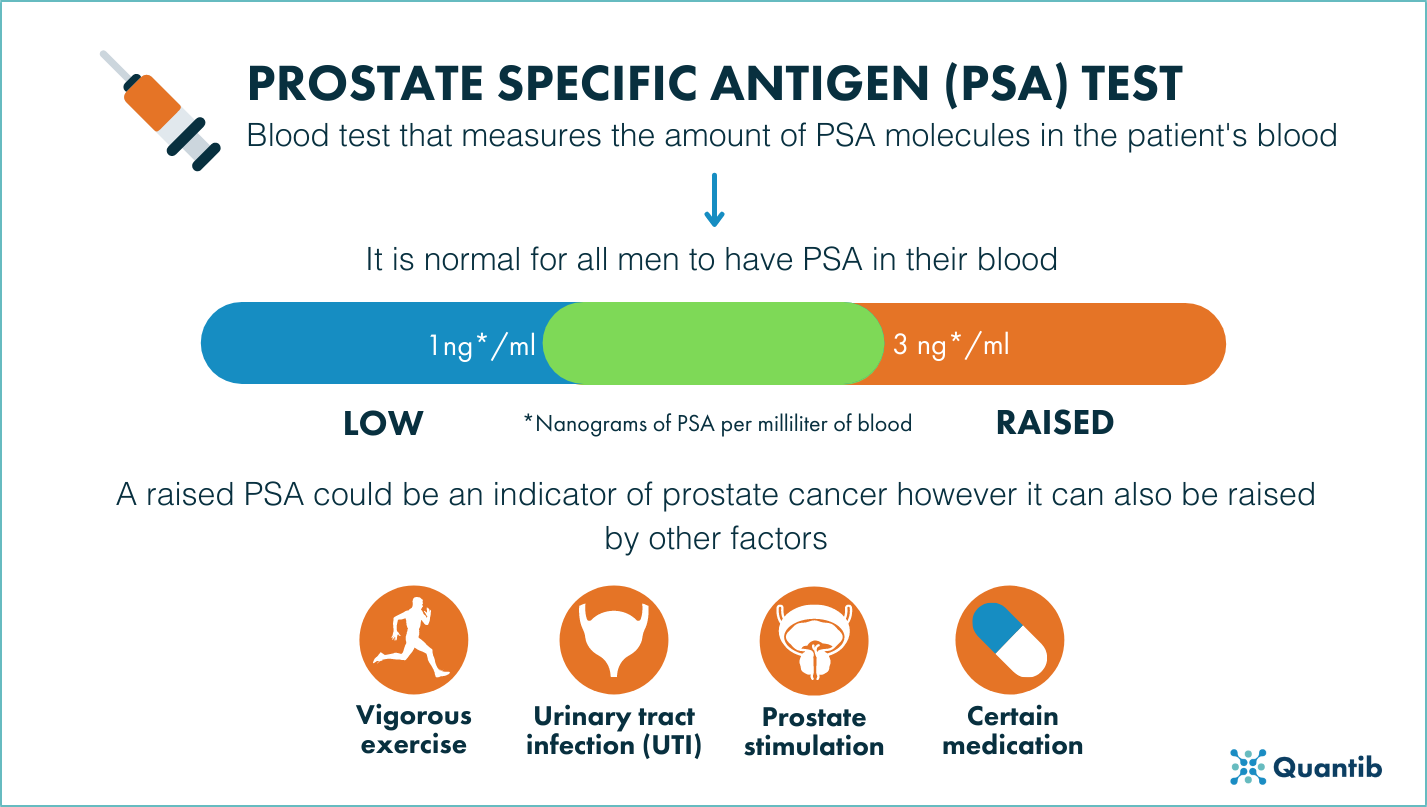
Figure 2: PSA test infographic.
Another example could be an infographic that details what is a prostate MRI and gives some tips for claustrophobic 4 patients, such as listening to music through headphones, in order to overcome how uncomfortable MRIs can be.
-
Detailed guides for the prostate cancer pathway
This asset differs from the infographic in that the detailed guide is a document of relatively long extension that covers a specific topic in-depth and the infographic is a summarized overview of a concept presented, primarily in a visual way.
For more invasive procedures, such as biopsies, a detailed guide might be a better way to explain patients everything they need to know about it. We recommend using a detailed guide for this particular test because the preparation before the biopsy and the after care are quite important for the accuracy of the test and the well being of the patient.
-
Cheat sheets for the prostate cancer pathway
Lastly, we recommend preparing some small cheat sheets to summarize information patients might want to look at multiple times. The primary example is a cheat sheet containing answers to the most frequently asked questions about a procedure, whether it is a test or a treatment.
We also recommend offering a small cheat sheet that explains the different Gleason scores for detected prostate cancer in biopsy samples.
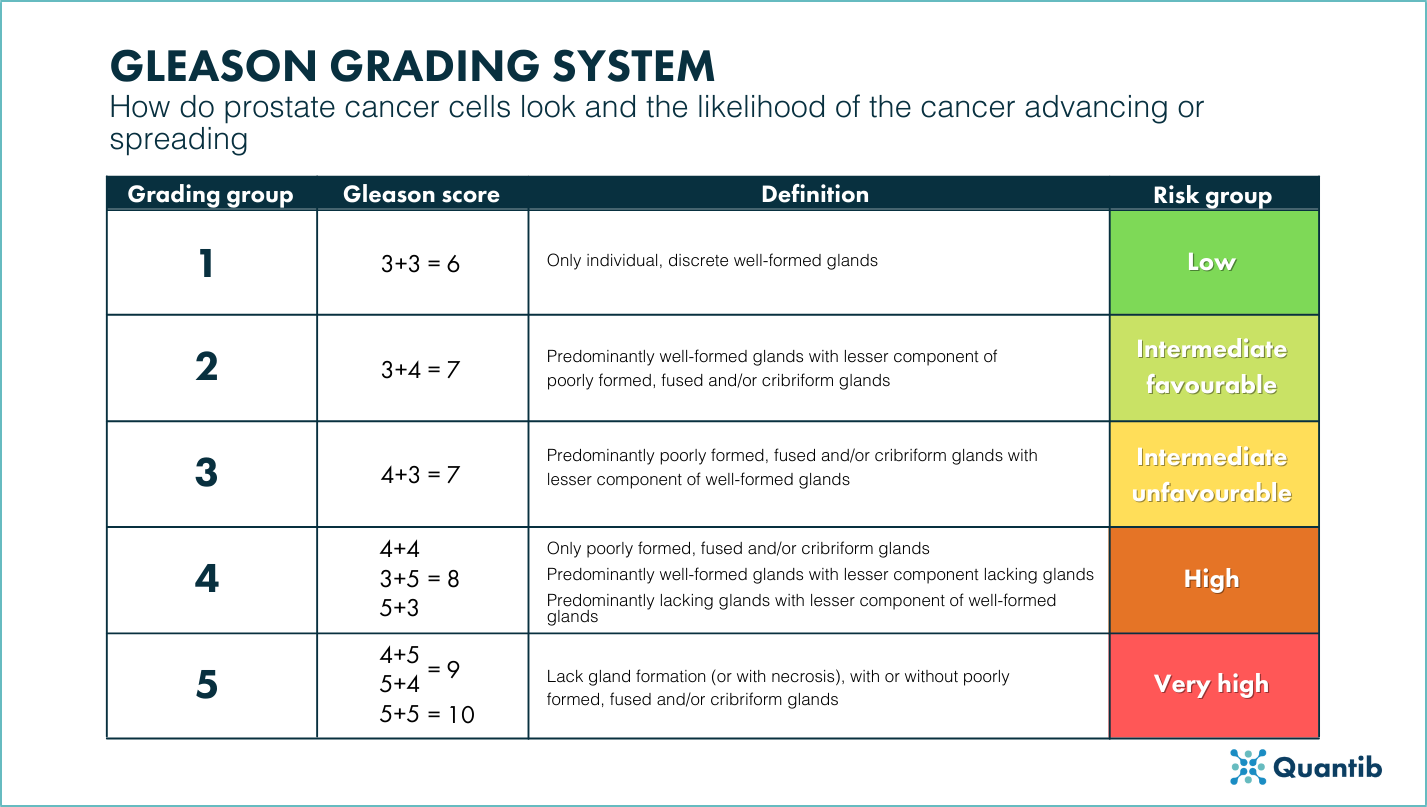
Figure 3: Cheat sheet of the Gleason grading system.
Consider active surveillance
Better safe than sorry goes in many situations and is definitely an approach to consider in the case of prostate cancer. A rigorous prostatectomy may be the right choice, however, it is an invasive procedure that may lead to devastating consequences because of potential side effects. Also, other treatment trajectories influence the live of patients severely, hence, considering and discussing active surveillance may be a good option more often than initially estimated 5.
Important soft skills for physicians involved in the prostate cancer pathway
The process can carry, as we have previously mentioned, a mental burden. Emotions can run high and can, therefore, exhaust the patient’s energy which he strongly needs for undergoing his treatment if it comes to that.
Detecting and managing these feelings are important soft skills for a physician to make the experience as bearable as possible for their patients.
Communication skills to support prostate cancer patients
No patient is the same and, therefore, they will not have the same expectations from the urologist when it comes to communication. Different types of patients require different approaches.
Does you patient want to be heavily involved and know every detail? Provide a lot of information and use, for example, the resources we discussed above to provide the patient with an overview of the situation, the different options for next steps and the pros and cons of those options. This will equip them with making the possibly hardest decision of their lives, let it be an informed one. Other patients rely heavily on the physicians expertise. To them, urologists are the expert and should be the patient’s beacon when it comes to all things related to their disease. Most likely, you do not want to overload these patients with information. They will want to know the essentials, possibly explained using clear and informative images, but mostly they are looking for their urologists to provide advice.
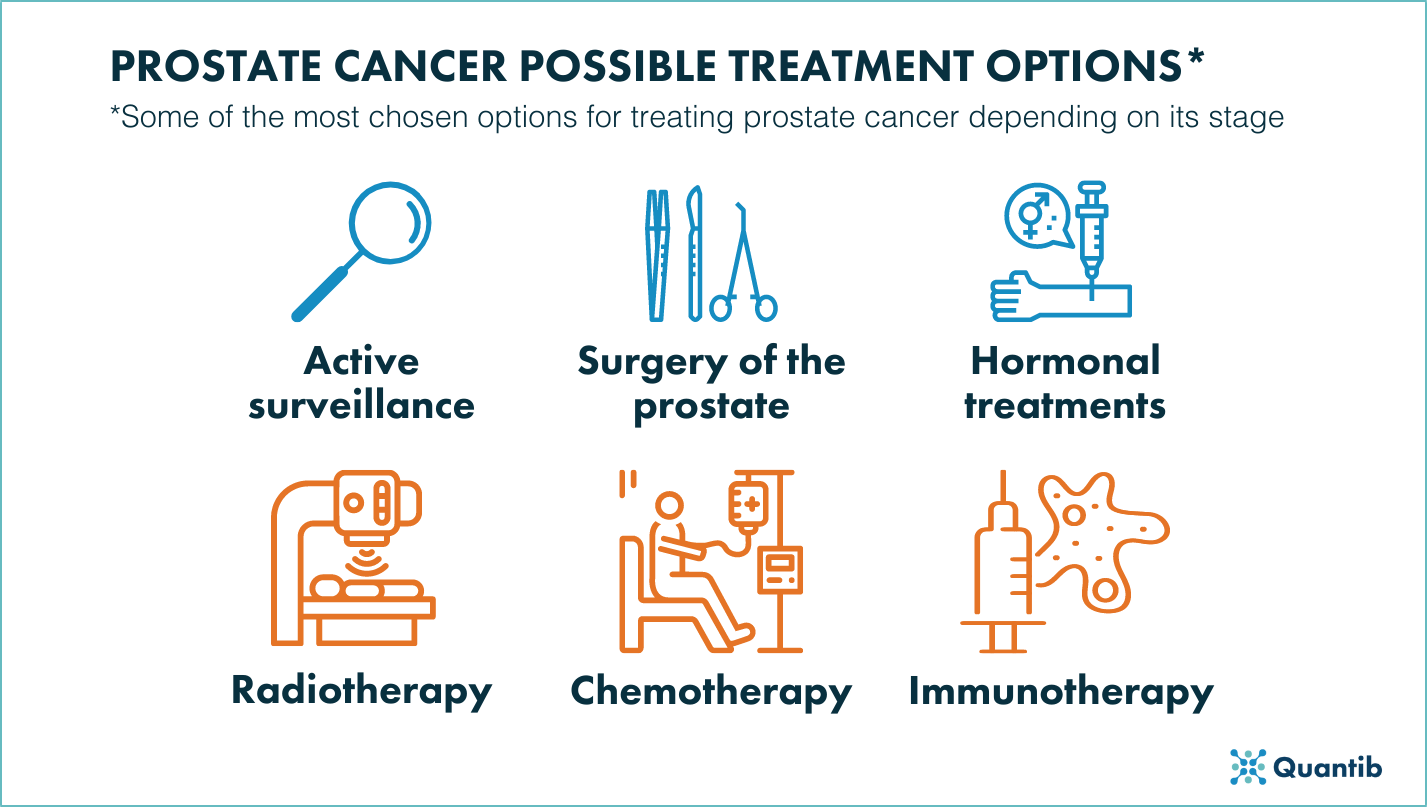
Figure 4: Summarized overview of the different treatment options to fight prostate cancer.
In retrospect, urologists might realize, after years of practice, that what patients value the most or makes them feel at ease, are professionals that answer their questions in a deep and through way and are caring towards them6,7. This shows the importance of being present as a urologist.
Empathy to support prostate cancer patients
Practiced urologists know like no other how important it is to be empathic during the whole prostate cancer diagnosis process. Empathy becomes even more important during the diagnosis and treatment choice phase when the news are negative for the patient. It is difficult enough to have to come to terms with the news of having prostate cancer and its consequences so it is imperative to be honest and refrain from giving false hope.
Listening skills to support prostate cancer patients
Being patient and listening to patients’ needs is another valued part of good communication. On one hand, they will feel valued and cared for and, on the other hand, it is the best way to personalize the care so that it fits their complaints and their wishes.
AI support
Patients may be quite restless while waiting for results. Certain solutions may help physicians deliver more accurate and faster results to fight that anticipation. For example, AI-driven solutions for reading prostate MRI.
AI-based solutions may be able support urologists providing improved patient care. They may reduce the turn around time for some of the results which will help counteract patients anxious feelings. Additionally, such a solution generally provides a standardized report that is not only easy to communicate, but also easy to understand. This will help patients to grasp what their results really mean and come to terms with them.
Other AI solutions can be applied to different parts of the prostate cancer diagnosis such as algorithms that calculate personalized risk associated with different treatment options or surgery support like 3D holographic image projection during the procedure.
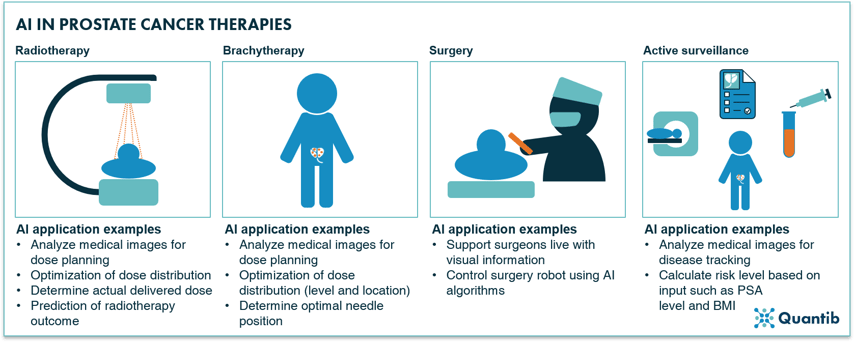 Figure 5: Radiotherapy, brachytherapy, surgery and active surveillance are amongst the most applied therapies for prostate cancer with a wide range of options for application of AI-based support.
Figure 5: Radiotherapy, brachytherapy, surgery and active surveillance are amongst the most applied therapies for prostate cancer with a wide range of options for application of AI-based support.
Conclusion
Improving the quality of patient care in the clinical pathway for prostate cancer is a responsibility of all physicians involved. Besides the medical knowledge, social skills, such as empathy or communication, are very important, one might even argue in some cases more important than the clinical competencies..
The use of digital or printed materials to support urologists communication with patients, such as infographics or cheat sheets, is highly recommended in order to improve the understanding of the procedures and the treatments patients might undergo.
Taking this into account, physicians will be able to improve patient centeredness and, with that, the overall experience of the patient with the whole clinical pathway of prostate cancer diagnosis.
Bibliography
- Delaney, L. J. Patient-centred care as an approach to improving health care in Australia. Collegian (2017) doi:10.1016/j.colegn.2017.02.005.
- Patient-centred care explained. https://www.betterhealth.vic.gov.au/health/servicesandsupport/patient-centred-care-explained/ (2015).
- Balkac, M. & Ergun, E. Role of Infographics in Healthcare. Chinese Medical Journal 131, (2018).
- Prostate Cancer UK. Prostate tests: MRI scam. https://prostatecanceruk.org/prostate-information/prostate-tests/mri-scan (2019).
- Wolinsky, H. Prostate Surgery and Outright Lies. MedPage Today https://www.medpagetoday.com/special-reports/apatientsjourney/73386 (2018).
- Rosevear, H. Residency vs. the real world: 5 things I wish I’d known. Urology Times https://www.urologytimes.com/view/residency-vs-real-world-5-things-i-wish-id-known (2019).
- UPMC. Patient Testimonials UPMC Urology of Central PA. https://www.urologycp.com/testimonials/ (2021).